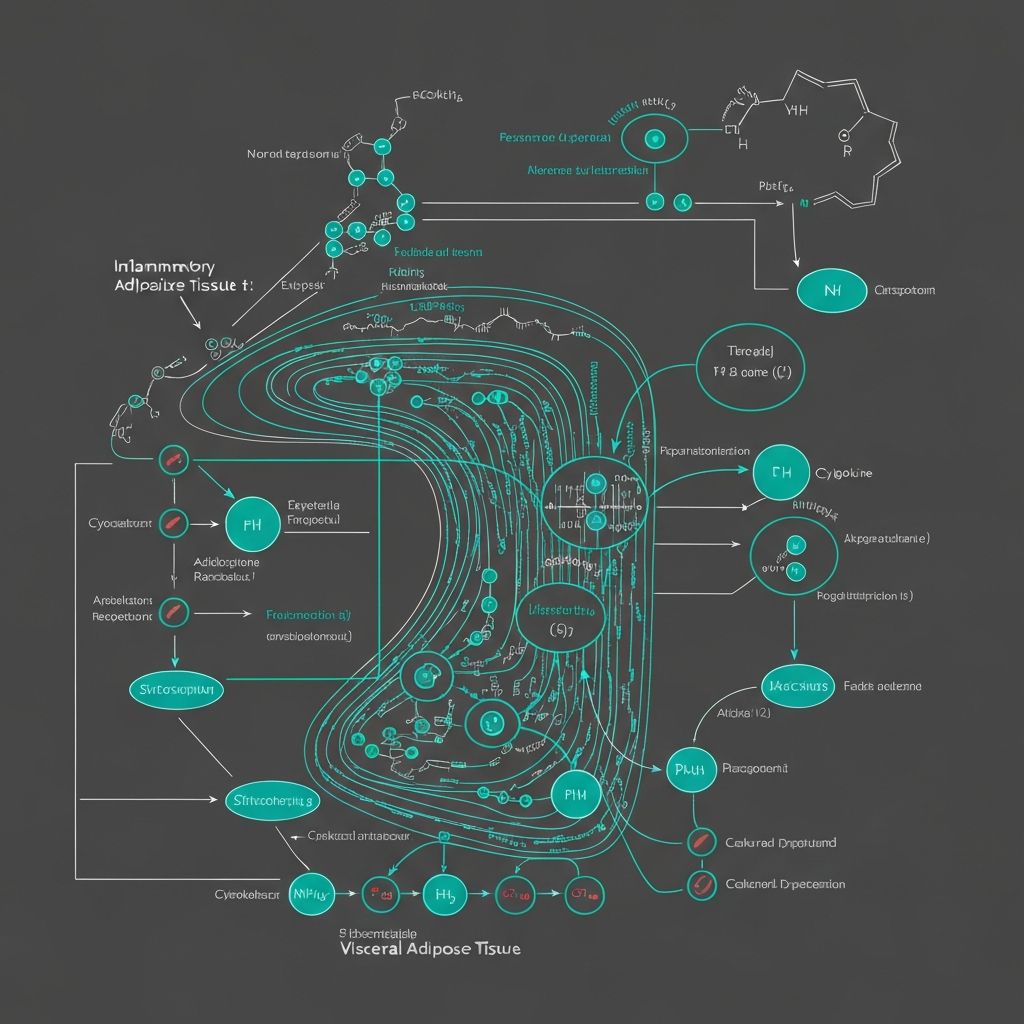
Inflammation and Adipokine Dysregulation in Visceral Obesity
Exploring the inflammatory environment of visceral fat and its metabolic consequences.
Chronic Low-Grade Inflammation in Visceral Adiposity
Visceral adipose tissue exhibits a characteristic chronic inflammatory state distinct from subcutaneous fat compartments. This low-grade systemic inflammation, sometimes termed metaflammation (metabolic inflammation), represents a central feature of visceral obesity and contributes substantially to metabolic dysfunction and systemic health consequences.
The inflammatory environment of visceral fat reflects several interconnected processes including elevated production of pro-inflammatory cytokines by adipocytes and infiltrating immune cells, increased oxidative stress within adipose tissue, altered metabolic milieu favoring inflammatory activation, and disrupted adipokine signaling promoting inflammatory cascades.
Pro-Inflammatory Cytokine Production
Visceral adipose tissue produces substantially higher concentrations of pro-inflammatory cytokines compared to subcutaneous depots. Key inflammatory mediators include:
- Interleukin-6 (IL-6) - produced by both adipocytes and infiltrating immune cells, circulates systemically and acts on liver and muscle
- Tumor Necrosis Factor-α (TNF-α) - potent pro-inflammatory cytokine contributing to insulin resistance and systemic inflammation
- Interleukin-1β (IL-1β) - contributes to inflammatory signaling and metabolic dysregulation
- Monocyte Chemoattractant Protein-1 (MCP-1/CCL2) - chemokine attracting immune cells to adipose tissue
These cytokines are released directly into the portal circulation, delivering inflammatory signals directly to the liver. Portal delivery of elevated pro-inflammatory cytokines impairs hepatic metabolic function and contributes to fatty liver disease development in visceral obesity.
Macrophage Infiltration and Immune Cell Composition
Visceral adipose tissue contains substantially higher numbers of infiltrating macrophages and other immune cells compared to subcutaneous depots. In obesity, adipose tissue macrophage content can increase 5-10 fold, creating a chronic inflammatory milieu within the tissue.
These infiltrating macrophages exist in activated states producing pro-inflammatory mediators. The macrophage-to-adipocyte ratio in visceral fat correlates with markers of inflammation and metabolic dysfunction. Interestingly, adipose tissue macrophage density increases disproportionately with visceral versus subcutaneous obesity, partly explaining the elevated inflammatory tone of central adiposity.
Oxidative Stress and Hypoxia
Visceral adipose tissue exhibits elevated oxidative stress (excess production of reactive oxygen species) compared to subcutaneous compartments. Several mechanisms contribute to this oxidative burden:
- Hypertrophied adipocytes develop localized hypoxia (low oxygen)
- Impaired mitochondrial function increases reactive oxygen species production
- Enhanced metabolic activity in visceral fat generates more oxidative byproducts
- Reduced antioxidant defenses in visceral adipose tissue
Oxidative stress itself promotes inflammatory activation and impairs insulin signaling, creating a self-perpetuating cycle promoting continued visceral adiposity and metabolic dysfunction.
Adipokine Dysregulation
Adipokines are endocrine hormones produced by adipose tissue that regulate systemic metabolic function. In visceral obesity, adipokine production becomes dysregulated with profound metabolic consequences:
| Adipokine | Visceral Obesity Pattern | Metabolic Effect |
|---|---|---|
| Adiponectin | Reduced production | Loss of insulin-sensitizing and anti-inflammatory effects |
| Leptin | Elevated with signaling dysfunction | Leptin resistance prevents satiety signaling |
| Resistin | Elevated production | Promotes insulin resistance |
| Visfatin | Elevated production | Inflammatory effects and metabolic dysfunction |
Lipid Accumulation in Peripheral Tissues
The combination of elevated portal free fatty acid delivery and impaired adipose tissue metabolic function in visceral obesity promotes lipid accumulation in liver and muscle. Hepatic steatosis (fatty liver disease) frequently accompanies visceral obesity, reflecting excessive lipid accumulation in hepatocytes.
This ectopic (abnormal location) lipid accumulation in non-adipose tissues is strongly associated with metabolic dysfunction. Muscle lipid content impairs glucose uptake and insulin signaling. Hepatic lipid accumulation impairs hepatic glucose production regulation and promotes further inflammatory activation within the liver.
Endothelial Dysfunction and Vascular Effects
The chronic inflammatory state of visceral obesity affects vascular function. Elevated circulating pro-inflammatory cytokines and endothelial dysfunction impair vasodilation, promote atherosclerosis development, and increase cardiovascular risk. Portal delivery of inflammatory cytokines particularly affects hepatic and mesenteric vascular function.
Cellular Senescence and Tissue Remodeling
Visceral adipose tissue in obesity demonstrates increased cellular senescence (cells that have stopped dividing but persist metabolically active). Senescent cells produce elevated inflammatory mediators and contribute to the overall inflammatory milieu. Additionally, visceral adipose tissue undergoes pathological remodeling with abnormal extracellular matrix deposition and reduced tissue compliance.
Systemic Inflammatory Consequences
The combination of elevated pro-inflammatory cytokine production and adipokine dysregulation in visceral obesity creates systemic inflammation measurable through circulating inflammatory markers including C-reactive protein (CRP), IL-6, TNF-α, and others. This systemic inflammation associates with numerous health consequences independent of total body fatness.
Systemic inflammation contributes to insulin resistance, impaired endothelial function, accelerated atherosclerosis, and activation of inflammatory pathways in numerous tissues. The metabolic dysfunction associated with visceral obesity partly reflects this systemic inflammatory state superimposed on the direct local effects of visceral adiposity.
Inflammation and Continued Central Fat Accumulation
Importantly, the inflammatory environment itself perpetuates further visceral fat accumulation through several feedback mechanisms. Pro-inflammatory cytokines enhance lipogenic gene expression in visceral adipocytes, suppress lipolysis, and promote further immune cell infiltration. This creates a self-reinforcing inflammatory cycle promoting continued visceral adiposity expansion and worsening of metabolic dysfunction.
Educational Note
This article explains inflammatory mechanisms in visceral adiposity based on research findings. Individual inflammatory responses vary substantially based on genetics, prior inflammatory history, and numerous other factors. This information is educational only and does not constitute medical or inflammatory assessment guidance.